Aging Well Long Island
Helpful tips for family caregivers
January/February 2018
Sometimes caring for a family member can be very tense. There are serious conditions, like a stroke, that become more likely as we age. There are potential problems, such as the misuse of prescription drugs. And then there are family relations and old family dynamics that can become more wearing than the actual tasks of providing care. This month we look at a few sources of tension for family caregivers and provide suggestions to help you diminish them—including a dose of laughter.
The role of humor in caregiving
 “Laughter is the shortest distance between two people.” So quipped comedian Victor Borge. And indeed, studies bear him out.
“Laughter is the shortest distance between two people.” So quipped comedian Victor Borge. And indeed, studies bear him out.
Laughter, especially when it’s a shared joke, creates a bond between people that generates a feeling of intimacy. Humor reduces tension and lowers stress. It also helps people to think more creatively and come up with more flexible solutions.
Caring for an aging family member can be pretty serious business: doctor’s appointments, errands to run, finances to juggle, critical decisions to make. Add to this the tendency of family members to have differing perceptions and opinions, and there is ample room for conflict.
The good news is that we are built to laugh. Kindergartners average 300 laughter episodes a day. Adults, by contrast, are stunningly deficient, with typically only 17 chuckles in 24 hours.
Tips for interjecting humor
Used with care, you can certainly improve relations with a bit of humor. Here are some tips to consider:
- Is everyone in on the joke? Is the funny comment something all of you will appreciate? The bonding occurs when the joke is shared. If it’s not funny to everyone present, then it’s more likely to alienate than bring you closer.
- Is there a hidden agenda? Some people use humor to express dissatisfaction. These little jibes actually hurt and build distrust. Be sure your intent is to share fun. Ridicule or sarcasm will only backfire.
- Could you offer an apology? If your comment doesn’t generate laughter, are you ready to say, “I’m sorry! I guess that wasn’t funny.”? If not, think twice before speaking.
The next time you feel tensions rising, consider a light-hearted joke. Perhaps do something silly. Or, you might make a joke about a peculiarity of yours. An unexpected shared laugh can derail a conflict and help get everyone back in sync.
Return to topDrug misuse
 Surprising but true: Adults over age 65 are candidates for drug overuse and abuse.
Surprising but true: Adults over age 65 are candidates for drug overuse and abuse.
Drug abuse is not common among elders. And it is often unintentional.
But the misuse of prescription drugs poses exceptional dangers.
Older adults are prescribed more drugs than any other age group. Roughly 80 percent of those over age 65 have multiple chronic conditions. These health issues can be emotionally, socially and physically challenging. Drugs are one way to cope. Hearing, vision, and memory problems also contribute to unintentional mix-ups in drug use.
The top three categories of the most commonly misused and addictive drugs are:
- Painkillers. More than 40% of older adults experience chronic pain. Opioids are frequently prescribed. Typically, these drugs create a pleasant state of euphoria. This may lead to the desire to take more, or to take them longer than necessary for the pain. Opioid use increases the risk of confusion, falls, fractures and delirium.
- Tranquilizers. Tranquilizers are often prescribed to address anxiety. They can also be used for sleep problems. Their calming effect can lead to cloudy thinking, slower reflexes and unsteady walking. This increases the risk of falls and can make dementia symptoms worse.
- Stimulants. These medications promote alertness and energy, and can bring on euphoria. They put the heart at risk, however, by increasing blood pressure and heart rate.
If your loved one is taking any of these potentially addictive drugs, watch for signs of trouble:
- The prescription running out early. This may indicate overuse.
- Multiple prescribing doctors or pharmacies. This is especially common with opioids.
- A sudden increase in problems with balance, sleep, and/or memory. These can be side effects of the medications themselves, or signs of drug misuse.
If you’re concerned, ask the prescribing doctors to each do a review of all prescription and over-the counter-drugs.
Return to topSigns of stroke or "TIA"
 A stroke is a disabling, and potentially deadly condition. A blood clot gets lodged in the brain, denying blood and oxygen to those cells. In a very short period of time, that part of the brain can be damaged permanently. Depending on the location of the clot, a stroke can impair functions such as speech, walking or memory.
A stroke is a disabling, and potentially deadly condition. A blood clot gets lodged in the brain, denying blood and oxygen to those cells. In a very short period of time, that part of the brain can be damaged permanently. Depending on the location of the clot, a stroke can impair functions such as speech, walking or memory.
A “TIA” (short for transient ischemic attack) is sometimes called a “mini-stroke.” TIAs involve small clots, or clots that get dislodged naturally and break up quickly. TIAs last only a few minutes, and usually do not cause permanent damage. Still, a TIA is an important event.
A TIA is actually a “warning stroke.” Roughly 35% of people who have a TIA go on to have a full stroke within a year. Nearly half of all people who have a full stroke report they had symptoms of a TIA a few days before.
Signs of a stroke or TIA
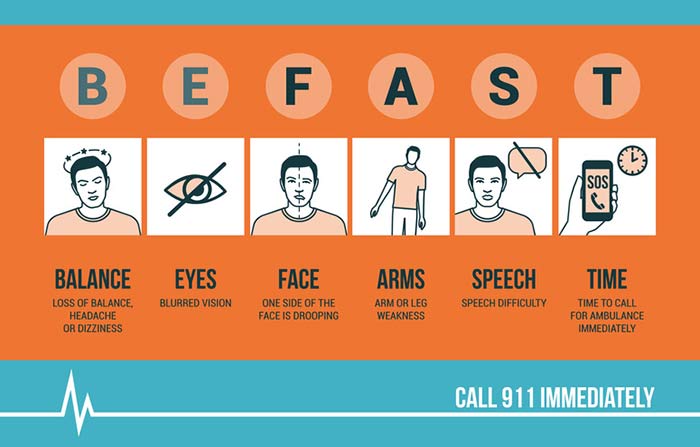
Because a clot can occur anywhere in the brain, symptoms can vary. Signs of a TIA or stroke are the same, and they come on suddenly. Recent research suggests you BE-FAST. Quickly size up the situation, looking for problems with:
- B-BALANCE: Sudden dizziness or loss of balance.
- E-EYES: Sudden blurriness or loss of vision in one or both eyes.
- F-FACE: Ask your loved one to smile. Does the smile look even? Does it look like their normal smile?
- A-ARM: Ask them to raise both arms. Does one arm drift down?
- S-SPEECH: Ask them to repeat a phrase. Does their speech sound slurred or strange?
- T-TIME: Every second without oxygen, brain cells die. Call 911 right away!
If you suspect your loved one is having a stroke or TIA, the best thing to do is call 911 immediately. Be ready to share the time you noticed the change, what signs you saw, and your loved one’s normal abilities.
Return to top
